Thank you
STOMACH
Prof. Jun Haeng LEE
Prof. Yong Hwan KWON
Prof. Woo Chul CHUNG
Prof. Seong Woo JEON
Dr. Yong Hwan AHN

CASE 1
CASE 2
CASE 3
CASE 4
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°In my GI endoscopy unit of hospital, there are 4 PENTAX Medical IMAGINA Video Endoscope Systems with 16 gastroscopes and 12 colonoscopes.
The first time IMAGINA system were installed in 2020, some endoscopists experienced minor difficulties in controlling the new endoscope due to some differences (e.g.: close position of the buttons, i-scan, feeling from the shaft, i-pad style touch panel, et al.) from existing ones of the other supplier.
But I easily get used to the PENTAX Medical IMAGINA endoscope system before long.
The major advantages of clinical case with IMAGINA are the excellent quality of close-up image and the function of high degree angulation. It is convenient to make high quality video clips using the 2 USB ports (please don't forget to use the most recent version of USB memory).¡±
Cascade Stomach
Patient History
Screening endoscopy of a 48-year-old female without any symptom and sign.
Endoscopic Findings
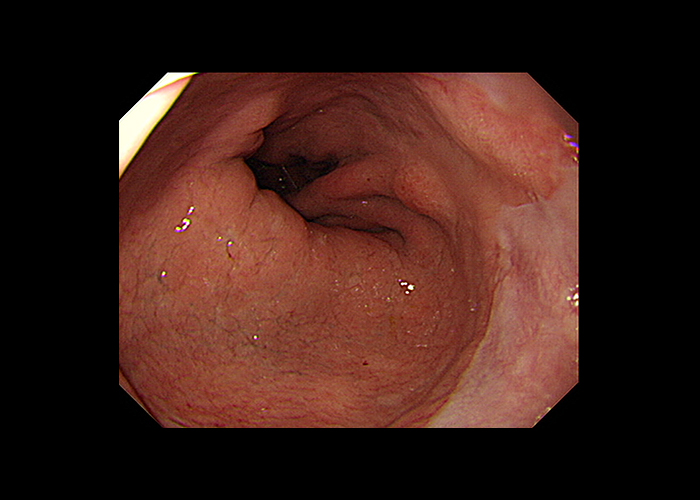
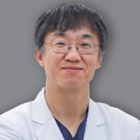
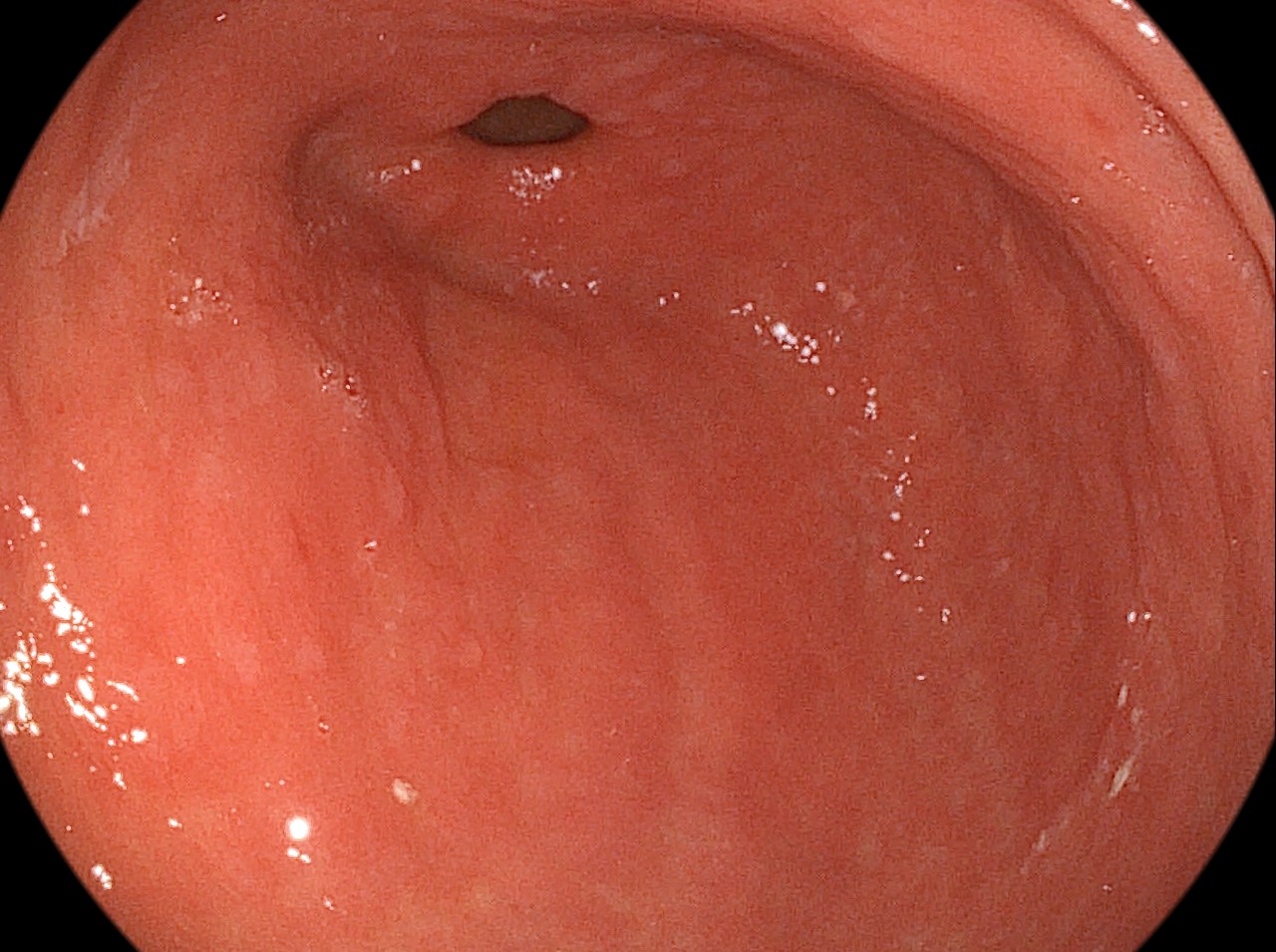
When the endoscope was introduced into the stomach, the lumen of the gastric body was seen at the upper right corner.
After infusion of some air into the stomach, a ridge between the gastric fundus and upper body can be seen.
The ridge runs from the posterior wall of the cardia toward the anterior wall of the stomach, crossing the greater curvature.
When the stomach has a prominent ridge between the fundus and high body, it is called as the cascade stomach (CS). The clinical significance of CS is still uncertain.
Image 1
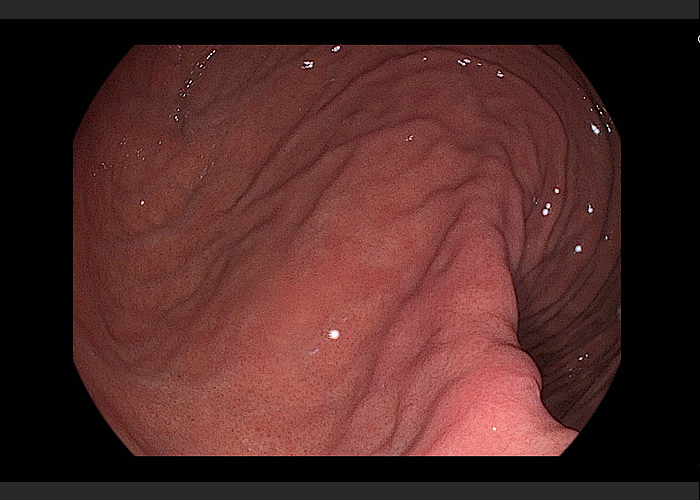
The timing of entering the stomach is very different between endoscopists.
Some endoscopists rapidly pass the esophagus without entering a lot of air.
In that situation, the stomach is not initially expanded at all.
For the other endoscopists, who carefully observe the esophagus before entering the stomach, there will be already an air in the stomach.
With a plenty of air in the stomach, the angulation between the fundus and high body can be changed, so the findings of Cascade stomach (a ridge between the gastric fundus and upper body) may be different.
In this case, the ridge runs from the posterior wall of the cardia toward the anterior wall of the stomach, crossing the greater curvature.
The clinical significance of this finding is unclear.
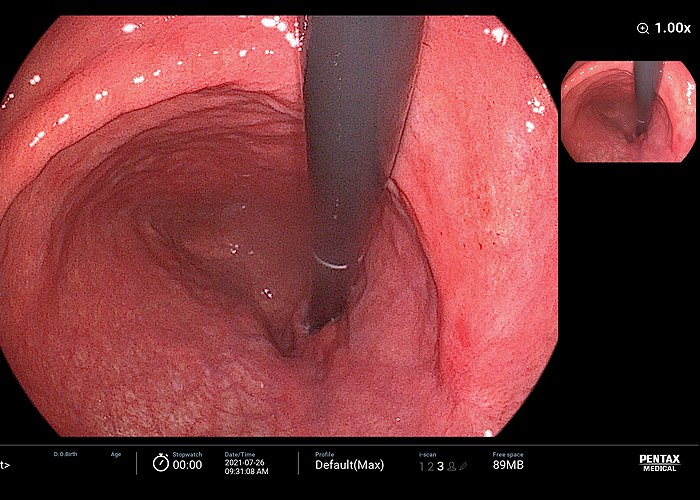
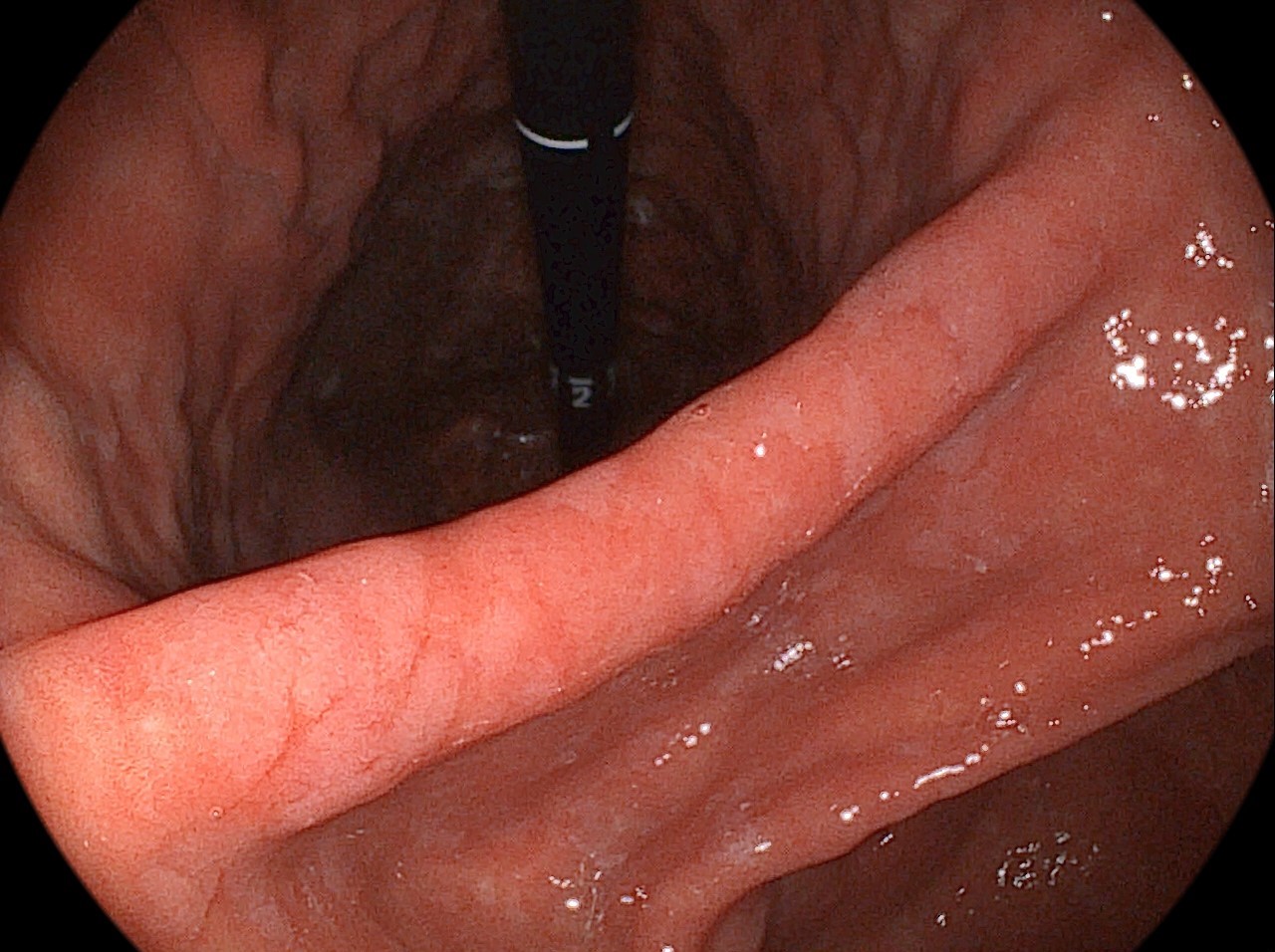
Image 2
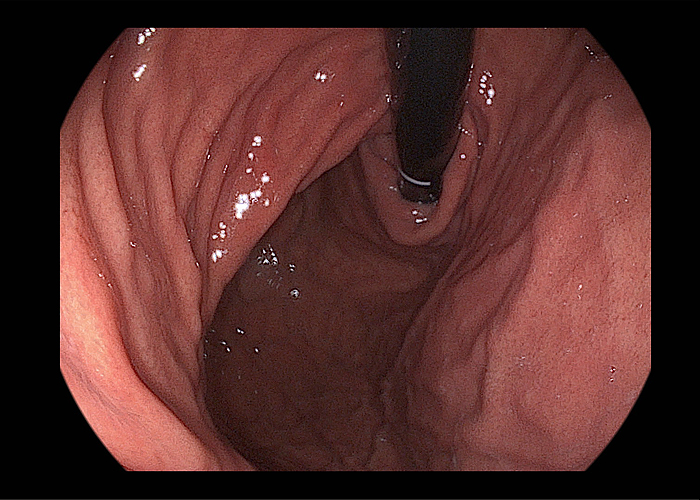
In this retroflection view, the ridge from the cardia is so prominent that I was not able to see the base of the fundus.
In this situation, it is quite easy to miss the lesion.
The base of the fundus and the posterior wall of the lower body are known as blind areas.
Before finishing the stomach observation, you need to rotate the endoscope counter-clockwise,
so that you can see the base of the fundus en face.
Image 3
Video clip available
Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°In my GI endoscopy unit of hospital, there are 4 PENTAX Medical IMAGINA Video Endoscope Systems with 16 gastroscopes and 12 colonoscopes.
The first time IMAGINA system were installed in 2020, some endoscopists experienced minor difficulties in controlling the new endoscope due to some differences (e.g.: close position of the buttons, i-scan, feeling from the shaft, i-pad style touch panel, et al.) from existing ones of the other supplier.
But I easily get used to the PENTAX Medical IMAGINA endoscope system before long.
The major advantages of clinical case with IMAGINA are the excellent quality of close-up image and the function of high degree angulation. It is convenient to make high quality video clips using the 2 USB ports (please don't forget to use the most recent version of USB memory).¡±
Advanced Gastric Cancer, Borrmann Type IV
Patient History
A 49-year-old female with symptom of early fullness and with the sign of weight loss.
Endoscopic Findings
The result of endoscopic forceps biopsy was poorly cohesive carcinoma.
Abdominal CT images showed diffuse wall thickening mass of the upper body and fundus of stomach with mild per-gastric infiltration.
The preoperative diagnosis was the advanced gastric cancer, Borrmann type IV.
Patient Outcome and Follow-ups
Surgical consultation was done for the exploratory laparotomy.
However, there were multiple seeding nodules found in the laparoscopy.
Palliative chemotherapy was done.
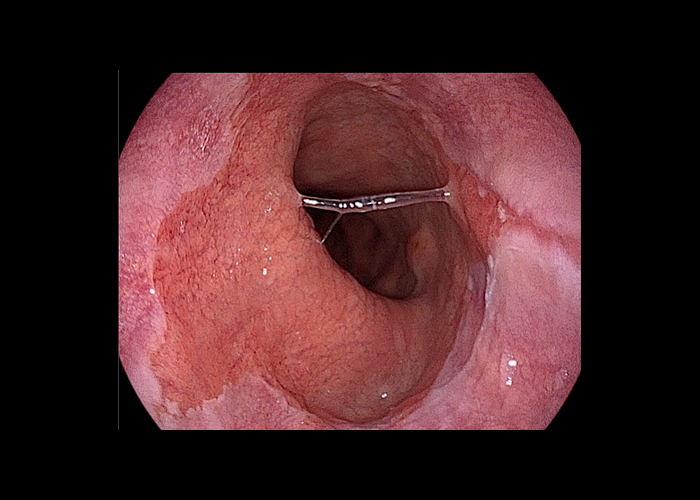
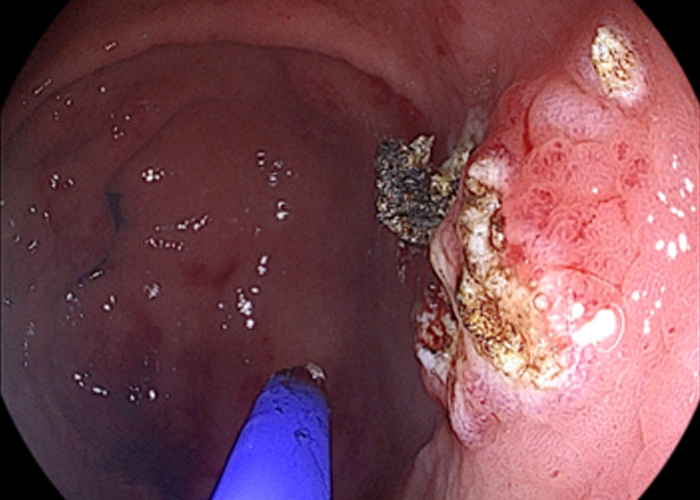
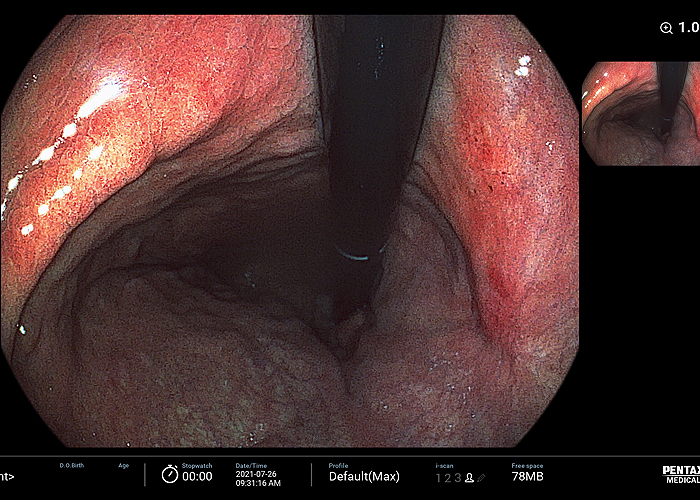
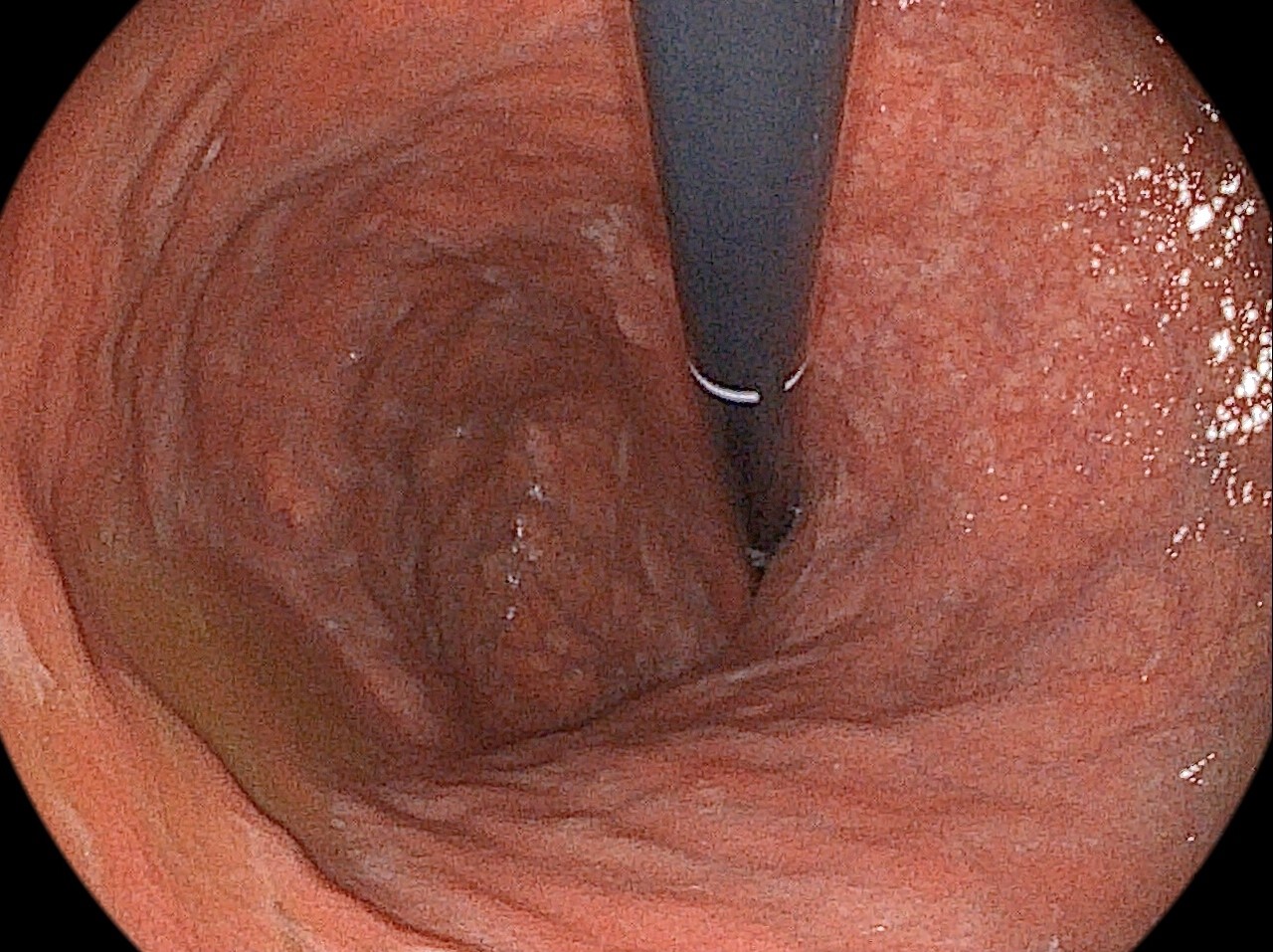
Image 1
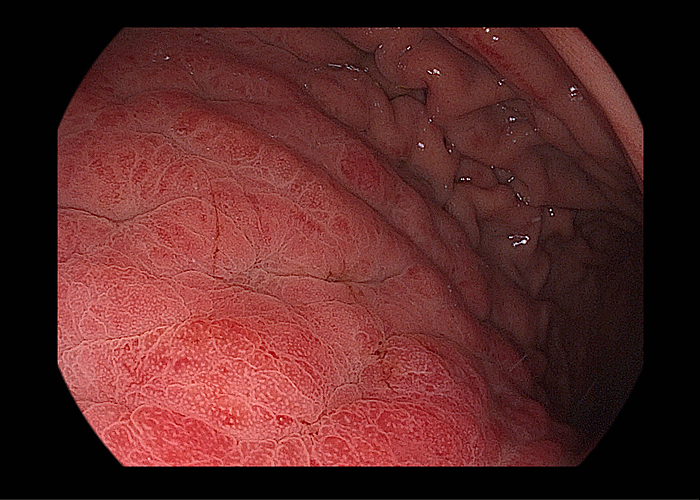
Image of the high body greater curvature and posterior wall:
The gastric folds are diffusely thickened.
The interval between folds was narrowed and some folds were conglomerated to form an ill-defined flat elevated area.
The surface was diffusely hyperemic and shows mosaic pattern, which means the accentuation of the normal area gastricae.
The lumen of the stomach was slightly expanded by air but not enough.
There was no definite ulcer or erosion.
Image 2
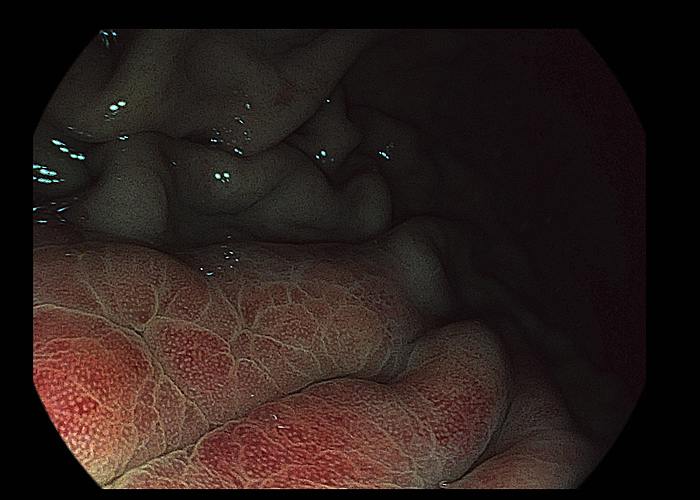
Image enhanced endoscopy by i-Scan:
The surface mosaic pattern is more clearly seen.
Image 3
Video clip available
Initially you can see the thickened folds and narrowed interval between folds.
The antrum does not seem to be involved by the diffuse type malignancy.
.
The border between the involved and normal areas looks
like somewhere between lower body and proximal antrum.
In the retroflection view, the whole area of the fundus and the cardia was involved.
There was no ulcer or erosion.
Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°PENTAX Medical IMAGINA i10c gastroscope was originally developed as a multifunctional upper endoscope not only for diagnosis but also for therapeutic purposes.
(1) It has a very wide working channel (inner diameter = 3.2mm), so suction of the air is available during the therapeutic procedures. Recent gastroscope models from other supplier have 2.8mm inner diameter on the working channel, which makes suctioning air with catheters in the working channel impossible.
(2) It has a waterjet function, so that irrigation during the procedure is possible. (There is one major limitation in this aspect. The water line is single use only.)
(3) The angulation is so good that the procedures for the lesions in the difficult locations are relatively easy and save times.
(4) The weight of the i10c scope is much decreased from the previous PENTAX version and relatively light in comparison with products from different suppliers. It may be an ideal endoscope for me, a therapeutic endoscopists in 50s looking for the ergonomic design to relieve the pain on shoulders and wrists."
APC Ablation for Adenoma
Patient History
A 68-year-old male with no symptom and sign (referred for the treatment of incidental gastric adenoma found in the screening endoscopy)
Endoscopic Findings
In the screening endoscopy, about 1.5cm sized ill-defined mucosal irregularity was found in the lesser curvature of the midbody.
Background gastric mucosal was atrophic.
Patient Outcome and Follow-ups
The biopsy showed adenoma with low grade dysplasia.
Ablation treatment using Argon Plasma Coagulation apparatus was done.
After treatment, PPI was given for two weeks.
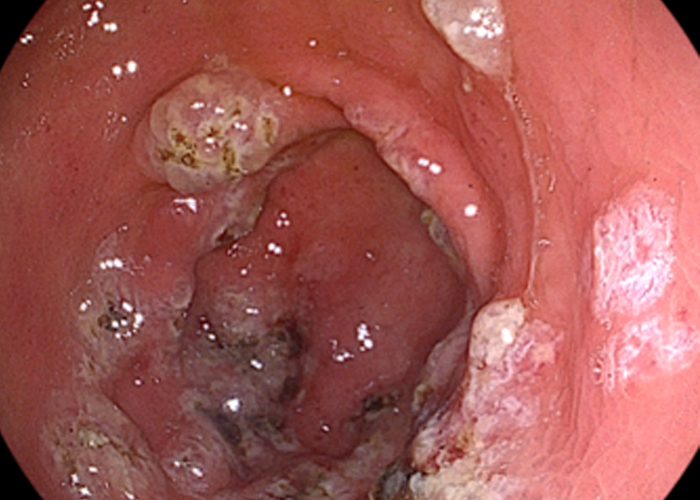
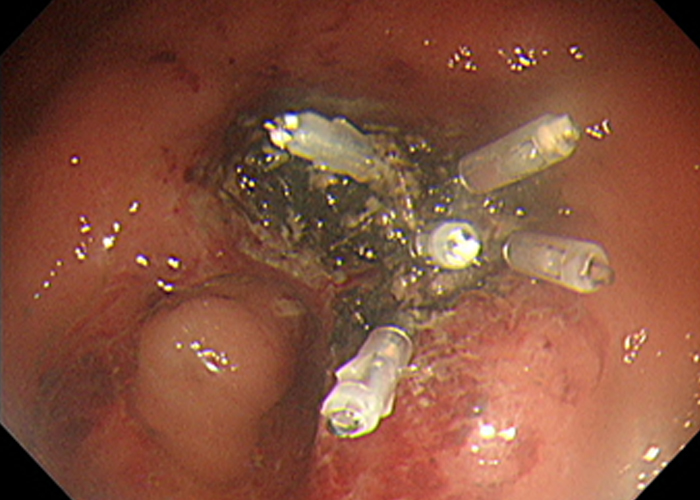
Image 1

i-scan image of the adenoma with low grade dysplasia in the lesser curvature of the lower body.
It is small, pale and flat, so endoscopic ablation can be an option.
Background gastric mucosa is atrophic.
Image 2
Just after ablation treatment with argon plasma coagulation (APC),
the lesion is changed into the white necrotic areas.
When you do follow-up endoscopy a few days later,
this lesion would be changed into a deep ulcer,
which is a mechanism of ablation treatment.
Image 3
Video clip available
Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°PENTAX Medical IMAGINA i10c gastroscope was originally developed as a multifunctional upper endoscope not only for diagnosis but also for therapeutic purposes.
(1) It has a very wide working channel (inner diameter = 3.2mm), so suction of the air is available during the therapeutic procedures. Recent gastroscope models from other supplier have 2.8mm inner diameter on the working channel, which makes suctioning air with catheters in the working channel impossible.
(2) It has a waterjet function, so that irrigation during the procedure is possible. (There is one major limitation in this aspect. The water line is single use only.)
(3) The angulation is so good that the procedures for the lesions in the difficult locations are relatively easy and save times. For gastric ESD cases, I choose Splash M-Knife, Splash M-Knife has lots of advantages during ESD. In the extended position of distal tip, there is a knife disk which can be hooked. I usually perform ESD using this hooking mechanism. The hooking mechanism is very useful for a lesions on difficult locations. Besides, Splash M-Knife has a superior hemostasis function. If the distal tip is in retracted position, distal tip and metal plate become like one body. By forming 1.5 cm or more round plate in this position, hemostasis is also possible and effective. When I perform submucosal injection in the middle of the ESD procedure, I don¡¯t need to change the knife and the procedure time is much saved due to the water jet function.¡±
ESD for EGC using Splash M Knife Only
Patient History
A 62 years old male patient visited my clinic due to a small gastric lesion found in the screening endoscopy.
Outside pathology report was 'tubular adenoma with high grade dysplasia, suspicious of adenocarcinoma'.
Outside pathology slide was reviewed by an in-house pathologist of Samsung Medical Center and the final pathology was 'adenocarcinoma, moderately differentiated¡¯.
The CT scan was negative for metastasis.
Endoscopic Finding, Treatment and Pathology Result
Stomach, EGC of proximal antrum, ESD with Splash M-Knife by PENTAX Medical
Location : antrum, greater curvature
Gross type : EGC type IIc+IIa
Histologic type : tubular adenocarcinoma, moderately differentiated
Histologic type by Lauren : intestinal
Size of carcinoma : longest diameter as 11 mm, vertical diameter as 10 mm
Depth of invasion : invades mucosa (muscularis mucosa) (pT1a)
Resection margin : free from carcinoma(N); safety margin : distal 14 mm, proximal 10 mm, anterior 10 mm, posterior 10 mm, deep 200 §
Lymphatic invasion : not identified(N)
Venous invasion : not identified(N)
Perineural invasion : not identified(N)
Microscopic ulcer : absent
Histologic heterogeneity: absent
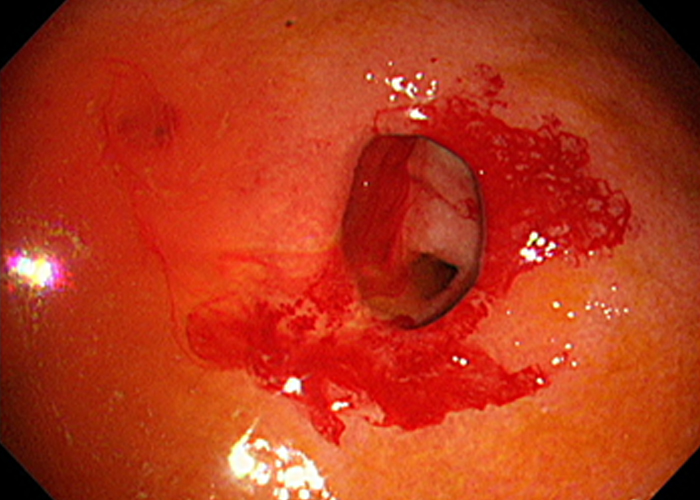
Image 1
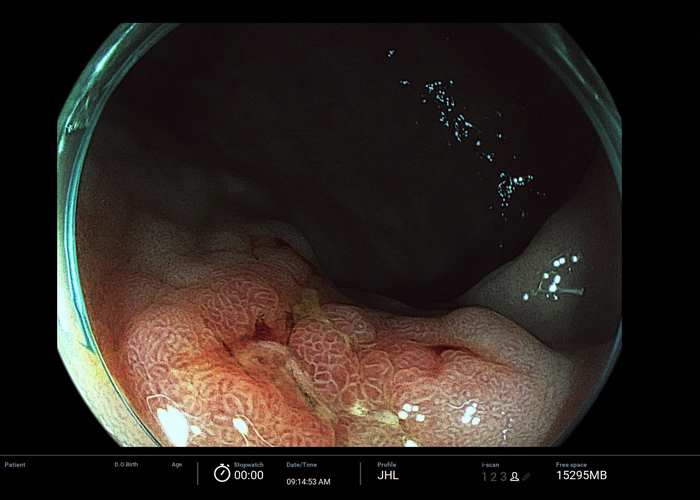
Image 2
ESU: ERBE VIO300D (mainly EndoCut I 3-3-3)
Bleeding control : Splash M-Knife (hemostatic forceps not used)
Sedation: Pethidine 25mg + Midazolam 5mg IV
Image 3
Video clip available
Summary
STOMACH
Prof. Jun Haeng LEE
Prof. Yong Hwan KWON
Prof. Woo Chul CHUNG
Prof. Seong Woo JEON
Dr. Yong Hwan AHN

CASE 1
CASE 2
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°HD+ and i-scan supported the characterization of the epithelial surface and vascularization of gastric mucosal lesions and can assist treatment and surveillance decisions.¡°
Gastric Adenoma
Patient History
A 74-year-old female was referred for the EGD through incidental finding on health examination.
Endoscopic Findings
20mm sized type IIa lesion at lesser curvature of mid-body.
i-scan SE and TE helped to demarcate the borders or the leision.
Endoscopic Treatment and Pathology Results
The lesion was dissected via gastric ESD.
The final pathology indicated early gastric adenoma, lower grade dysplasia.
Patient Outcome and Follow-ups
The lesion was resected en-bloc. During the procedure, no major bleeding occurred and no perforation could be spotted.
Image 1

Image 2
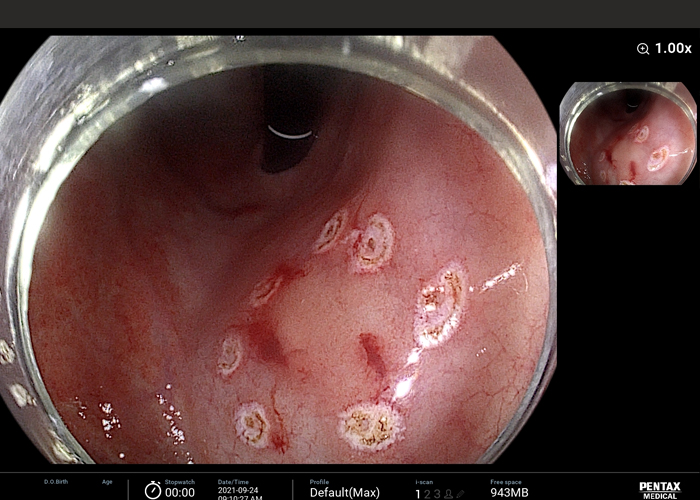
Image 3
Video clip available
Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡° I used the PENTAX Medical IMAGINA when the gastric ulcer bleeding was suspected.
The i-scan mode can help to discriminate whether the morphology of ulcer is benign or malignant based on change of color, vascularity and pit-pattern.¡°
Aspirin Induced Benign Gastric Ulcers
Patient History
A 78-year-old female visited emergency room for 3 days melena.
The patient had previous angina history and took aspirin for several years. Laboratory finding
Endoscopic Findings
CBC WBC 8600/§ Hb 8.7g/dL Hct 27% Plt 114K/§¡ Chemical and electrolyte battery Protein/Alb 6.6/3.8 g/dL AST/ALT 23/28IU/L ALP 96 U/L TB/DB 1.2/0.8mg/dL BUN/Cr 30.2/1.2 mg/dL Na/K 137/3.6 mmoL/L ESR 22mm/hr CRP 1.3mg/dL
Endoscopic Findings
The noted multiple ovoid ulcers surrounded with edematous mucosa at antrum, however, no active bleeding was seen in endoscopic finding.
The ulcers were shown smooth and regular shapes, even bases, clearly demarcated and regular edges.
The ulcer stage was A2 by Sakita-Miwa classification.
Patient Outcome and Follow-ups
Benign gastric ulcer and CLOtest (-)
Image 1
Video clip available
Summary
STOMACH
Prof. Jun Haeng LEE
Prof. Yong Hwan KWON
Prof. Woo Chul CHUNG
Prof. Seong Woo JEON
Dr. Yong Hwan AHN

CASE 1
CASE 2
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°IMAGINA video endoscope is suitable for therapeutic endoscopy and the image was sharper and crisper without losing focus. I can practice IMAGINA for various therapeutic endoscopy cases. Prejudice about PENTAX Medical endoscopes can be released I think.¡±
Gastric Adenoma
Patient History
A 73-year-old male with no medical history was referred for the endoscopic evaluation.
Endoscopic Findings
Large sliding hernia with erosive esophagitis (LA classification B) and 0.7cm sized sessile elevated mucosal lesion (Yamada type I polyp) were observed.
Endoscopic Treatment and Pathology Results
The microsopic diagnosis was gastric epithelial dysplasia – low grade.
Patient Outcome and Follow-ups
Annual endoscopic surveillance with biopsy.
Image 1
By endoscope of ¡®O¡¯ brand
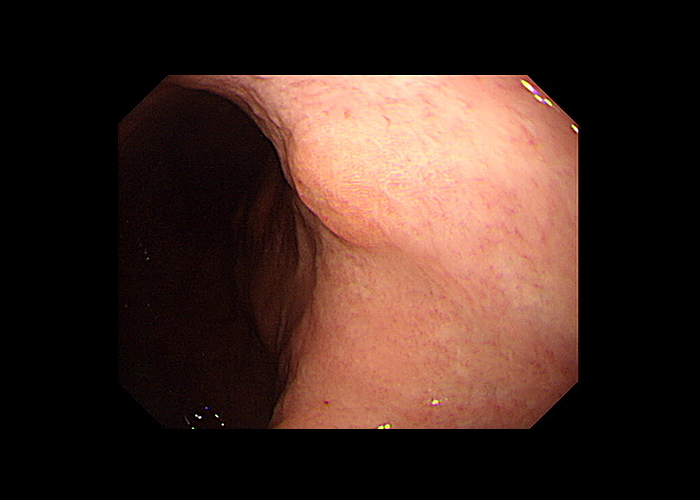
Image 2
By endoscope of PENTAX Medical IMAGINA

Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°During a case of endoscopic hemostasis with APC for the gastric angiodysplasia, there was no losing image quality from the argon smoke.
The near focus image was clearly visualized.¡°
Comparison of endoscopic hemostasis with PENTAX Medical IMAGNA (A) and the other company¡¯s endoscopy (B)
Active Bleeding in Gastric Angiodysplasia
Patient History
A 73-year-old male patient with hypertension was referred for taking out foreign matter (drug package) which was swallowed together with medicine.
Endoscopic Findings
The drug package was observed at mid esophagus. We used a protective device - endoscopic cap, in order to avoid esophagogastric/pharyngeal damage during endoscopic extraction of sharp-pointed foreign body. (image 1)
Successful removal and laceration wounds were observed. (image 2)
Endoscopic Treatment and Pathology Results
Foreign body removal by endoscopy
Patient Outcome and Follow-ups
The procedure performed successfully without any event.
Image 1
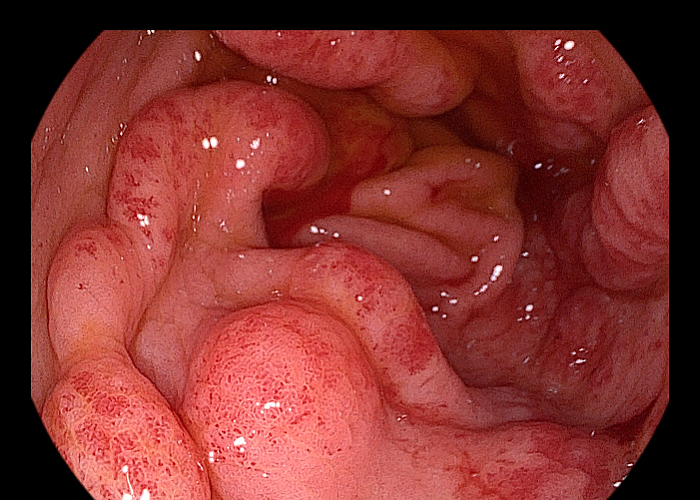

Image 2
Summary
STOMACH
Prof. Jun Haeng LEE
Prof. Yong Hwan KWON
Prof. Woo Chul CHUNG
Prof. Seong Woo JEON
Dr. Yong Hwan AHN
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡°I use PENTAX IMAGINA in daily clinical endoscopy practice. One of our endoscopy purpose is surveillance after endoscopic resection of gastric dysplasia or cancer.
The local recurrence is one of important subjects in follow up endoscopy. This could be diagnosed with endoscopic biopsy usually,
but as a therapeutic endoscopist, it is important to define the candidates for repeat ESD in the case of recurrence.
I assume that PENTAX IMAGINA TE mode is useful in this aspect. The PENTAX IMAGINA system have clear resolution and it can let me help the clear diagnosis. ¡°
Endoscopic Delineation of Early Gastric Cancer
Patient History
The patient is a 74-year-old female with a history of undergoing endoscopic submucosal dissection (ESD) in other hospital.
The initial diagnosis was early gastric cancer of moderately differentiated adenocarcinoma with 10mm in size and uncertain resection margin.
She was transferred to out center to ask second opinion for additional surgery.
I recommend her following up endoscopy to check recurrence of cancer.
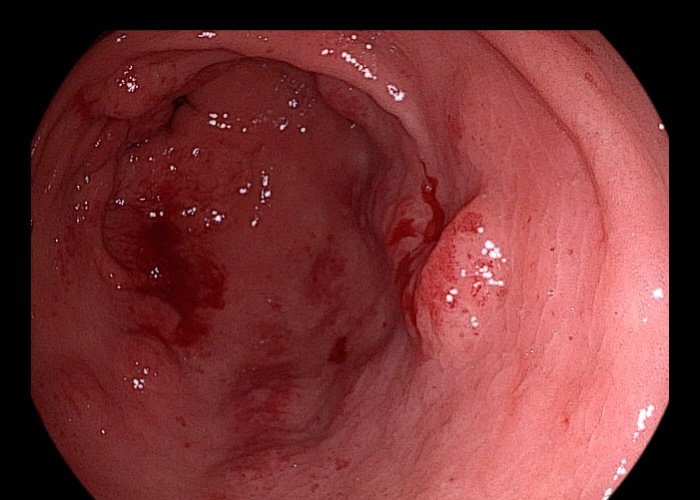
Endoscopic Findings
The endoscopic findings took 3months after ESD showed post ESD ulcer scar at LC of MB.
Also there noted slightly hyperemic ill-defined type llb lesion at PW of MB.
The biopsy revealed high grade dysplasia or well differentiated adenocarcinoma.
Endoscopic Treatment and Pathology Results
Repeat ESD was planned for the treatment of recurrent tumor.
The patient underwent gastric ESD 2 weeks later.
There was no complication related to this procedure. Final pathology was mucosal confined well differentiated adenocarcinoma,
measuring 4cm in maximal diameter.
Patient Outcome and Follow-ups
Regular EGD follow up would be provided to the patient.
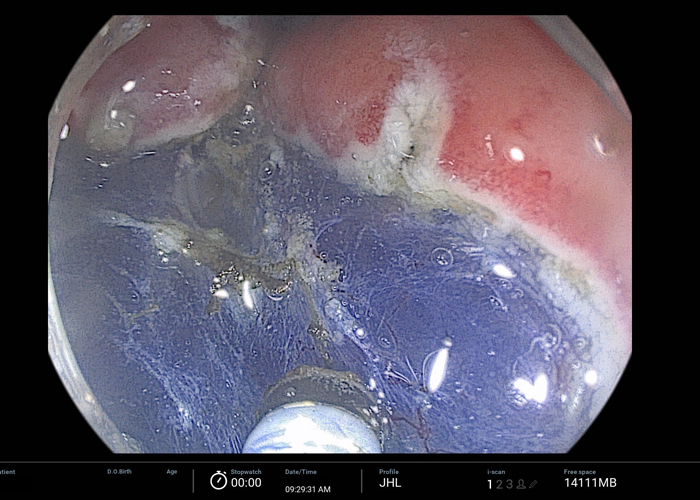
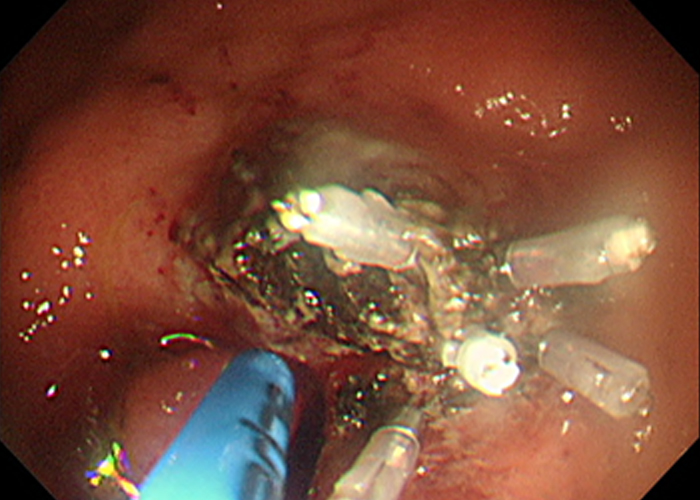
Image 1,2 & 3
The endoscopy findings with i-scan SE shows that post ESD ulcer scar at LC of MB.
The adjacent mucosa at posterior site had surface hyperemia and loss of regular pit pattern.
The size of the lesion was not definite on SE image (image 2),
and the margin of the lesion was uncheckable due to ill-defined border.
However, the i-scan TE shows clear margin with enhanced reddish mucosal lesion (image 3).
This could help define the exact border of the lesion and achieve curative resection.
Summary
STOMACH
Prof. Jun Haeng LEE
Prof. Yong Hwan KWON
Prof. Woo Chul CHUNG
Prof. Seong Woo JEON
Dr. Yong Hwan AHN

CASE 1
CASE 2
CASE 3
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡° Currently, I have been performing endoscopy of the stomach and colon using PENTAX Medical IMAGINA system for about 2 years. Previously, PENTAX Medical EPK-i video endoscope was used for examination. IMAGINA system exhibits more vivid colors and lighter handling, and it is easier to detect mucosal changes in close-up than any other system. In terms of color, images are reproduced without any visual burden, and this provides natural images when I explain the endoscopic findings directly to patients.¡°
Autoimmune Gastritis
Patient History
A 50-year-old female patient had intermittent postprandial discomfort for several years. She was taking medication for hypertension and hyperlipidemia. She denied a history of gastric acid secretion inhibitor use or treatment of Helicobacter pylori.
Endoscopic Findings
| Serologic tests | Patient |
|---|---|
| Pepsinogen I | 5.3 |
| Pepsinogen II | 11.0 |
| Pepsinogen I/II | 0.5 |
| Gastrin (13 ~ 115 pg/mL) | 365 |
| Anti-H. pylori IgG (0.0 ~ 0.89 U/mL) | 0.69 |
| Rapid urease test | Positive |
Endoscopic Finding & Biopsy
Autoimmune gastritis was suspected due to corpus predominantly severe atrophic gastritis on endoscopy, and a biopsy was performed to confirm the diagnosis. Biopsies were performed in the greater curvature of the upper gastric body and the greater curvature of the pyloric antrum (2cm proximal to the pyloric ring). Histological examination revealed normal gastric mucosa in the antrum and marked infiltration of inflammatory cells in the laminal propria and focal intestinal metaplasia in the upper body.
Patient Outcome and Follow-ups
The patient additionally had serum tests for anemia, thyroid function, vitamin B12, and vitamin D performed, and there was no specific findings. The patient is prescribed prokinetics for the symptoms, and regular endoscopy follow-up at 2-year interval is recommended.
Image 1
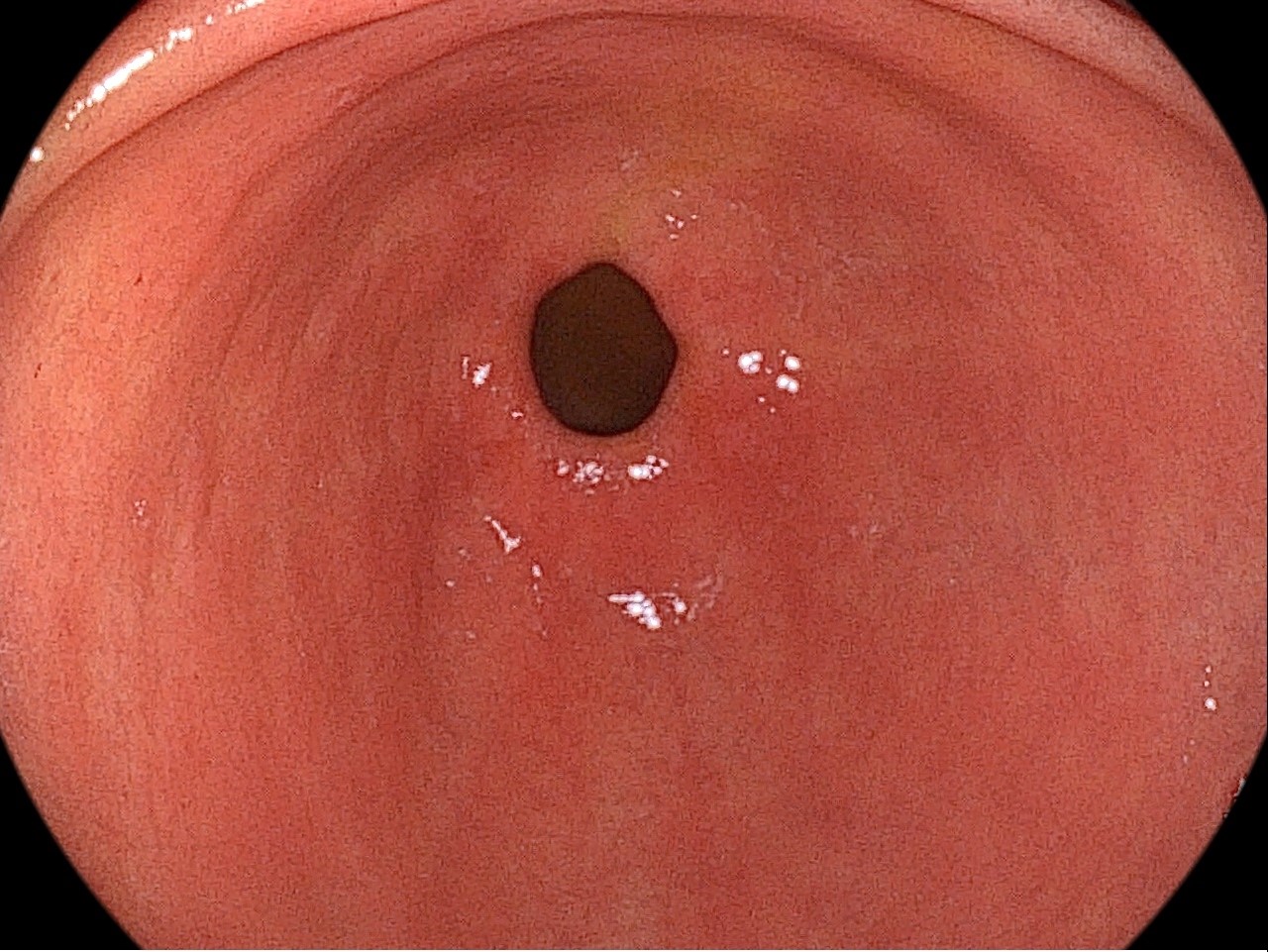
Normal gastric mucosa is observed in the antrum.
Image 2

Extensive atrophic changes with marked submucosal vasculature are
observed in the mucosa of the gastric body.
Image 3
Initially the normal gastric antrum is seen. However,
video endoscopic examination with retroflexion showed severe atrophic
changed mucosa of body and fundus. As a result of observation from the
antrum to the body, corpus of predominantly severe atrophic gastritis is
showed.
Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡° Currently, I have been performing endoscopy of the stomach and colon using PENTAX Medical IMAGINA system for about 2 years. Previously, PENTAX Medical EPK-i video endoscope was used for examination. IMAGINA system exhibits more vivid colors and lighter handling, and it is easier to detect mucosal changes in close-up than any other system. In terms of color, images are reproduced without any visual burden, and this provides natural images when I explain the endoscopic findings directly to patients.¡°
Autoimmune Gastritis with Subepithelial Tumor
Patient History
A 77-year-old female patient visited hospital for a follow-up examination for gastric subepithelial tumor. She complained about intermittent indigestion and often felt lethargic and weakness. She was taking antihypertensive drugs and having no history of taking other gastric acid secretion inhibitors.
Endoscopic Findings
| Serologic tests | Patient |
|---|---|
| Pepsinogen I | 10.1 |
| Pepsinogen II | 16.5 |
| Pepsinogen I/II | 0.6 |
| Gastrin (13 ~ 115 pg/mL) | > 1000 |
| Anti-H. pylori IgG (0.0 ~ 0.89 U/mL) | 0.42 |
| Anti-parietal cell ab. | Positive |
| Rapid urease test | 133.0 |
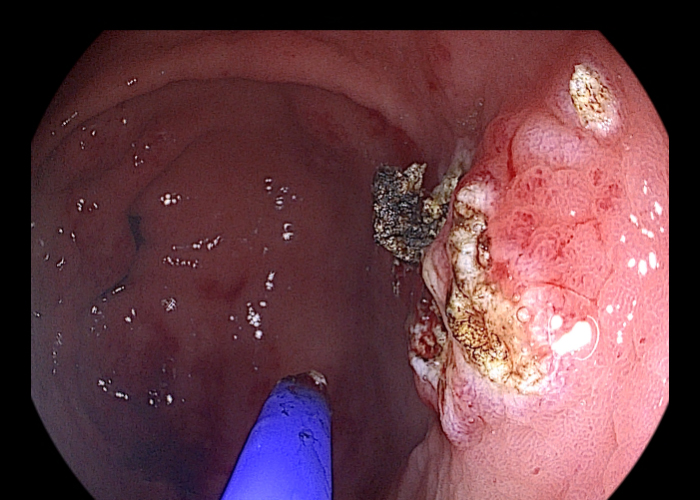
Endoscopic Findings
Endoscopy was performed about 2 years ago observing a 1.2cm subepithelial tumor in the fundus (Image 1). In a recent endoscopy, the tumor was observed to be about 2.5cm in size, grown to more than twice (Image 2). In terms of endoscopy, typical reverse atrophy was observed (Image 3, 4), and autoimmune gastritis was diagnosed through serological and histological findings.
Patient Outcome
I recommended treatment for a subepithelial tumor and transferred to a tertiary hospital. Prokinetics were prescribed for recovery of dyspepsia and cyanocobalamin was prescribed to relieve vitamin B12 deficiency.
Image 1
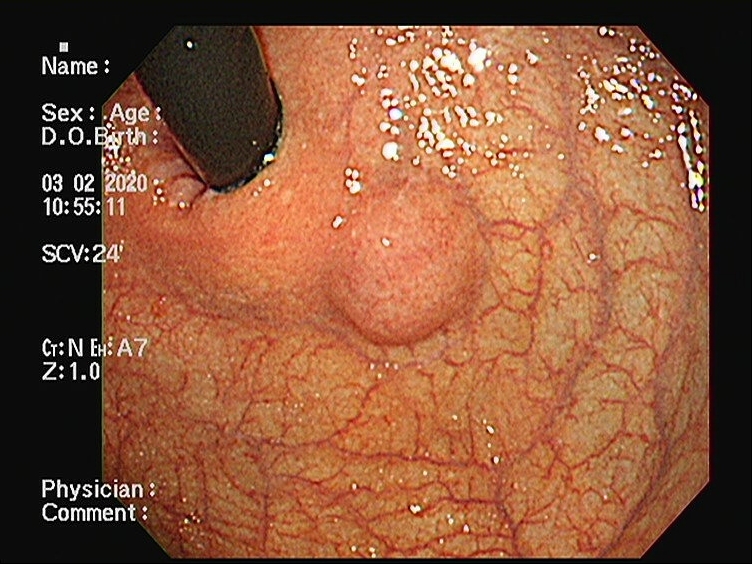
In the endoscopic image from another hospital taken 2 years ago,
a subepithelial tumor of about 1.2cm in size was seen in the fundus.
Image 2
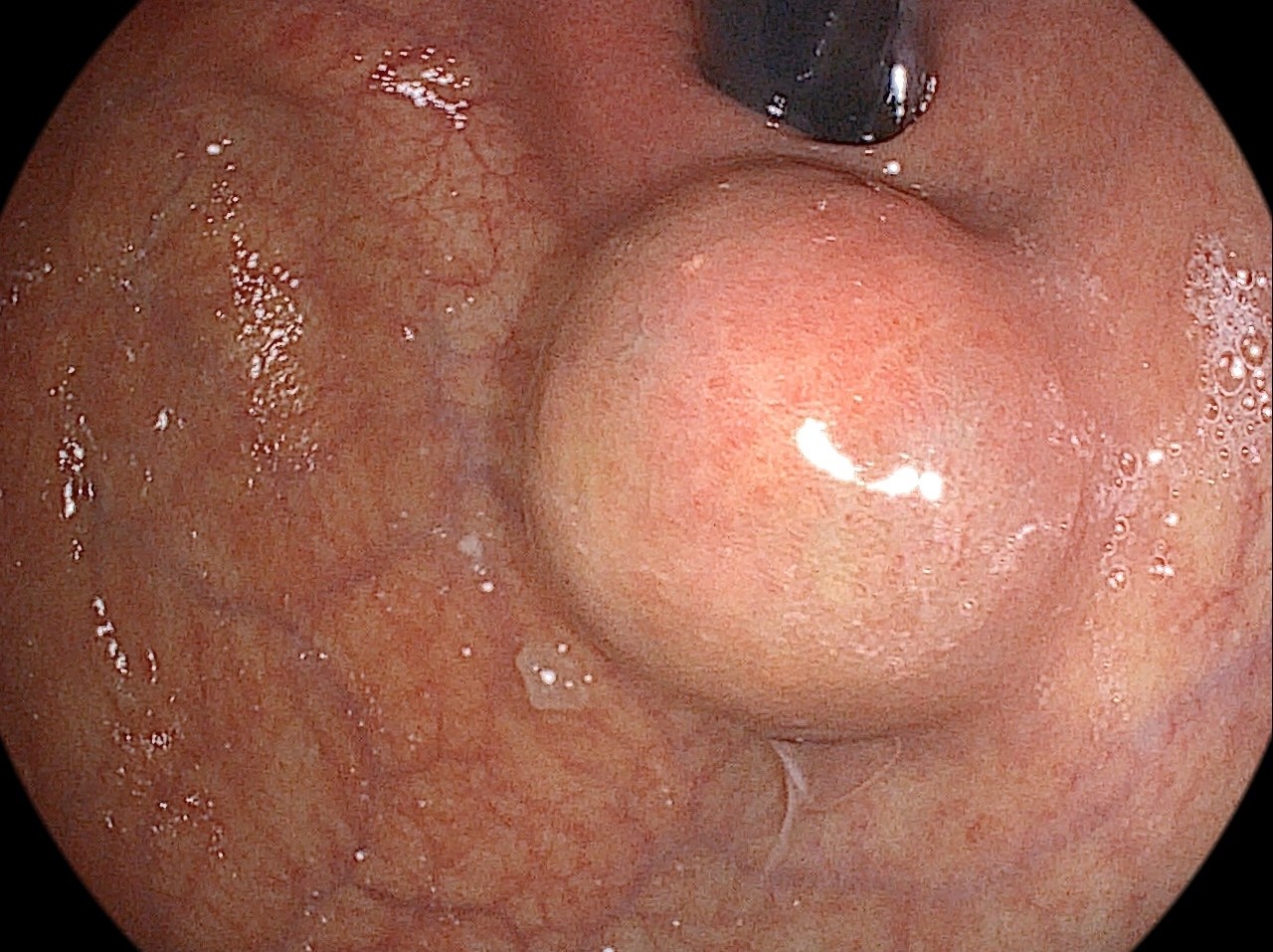
The subepithelial tumor of the fundus was enlarged to about 2.5cm in size.
Image 3
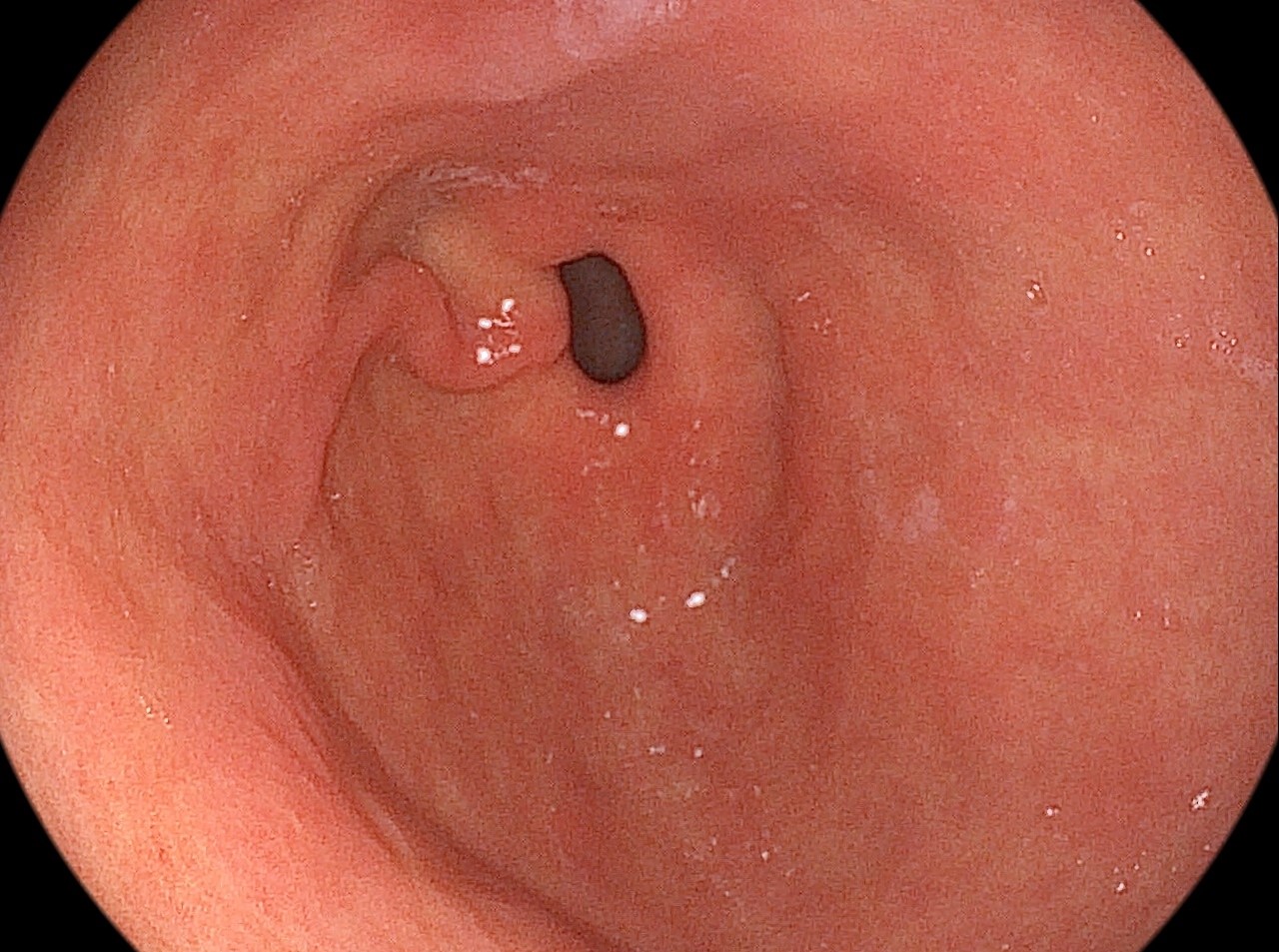
Normal gastric mucosa is observed in the antrum.
Image 4
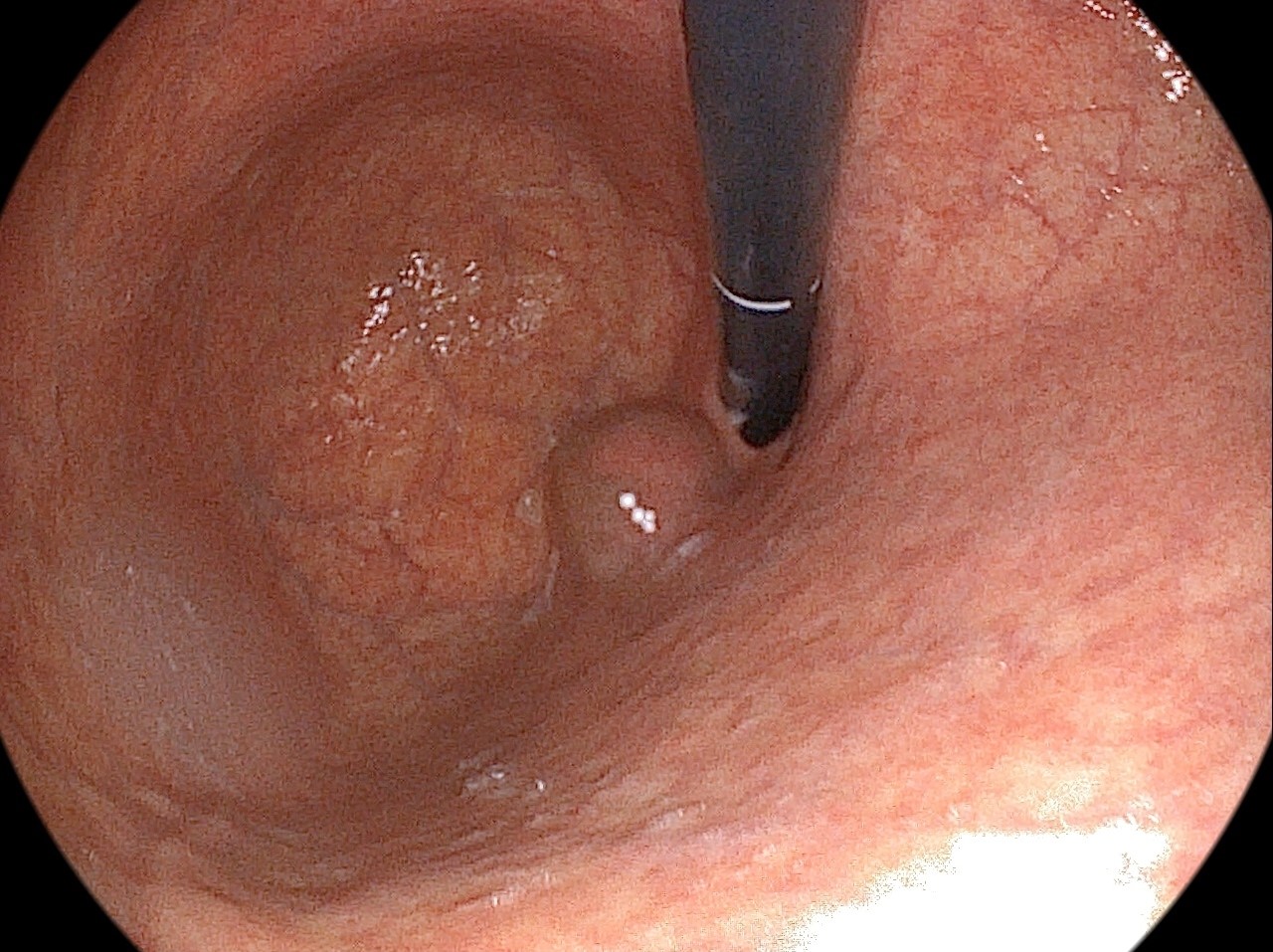
Endoscopy of retroflexion enables observation of severe mucosal atrophy with distinct submucosal vasculature in the body and fundus.
Summary
How do I use PENTAX IMAGINA in my clinical endoscopy cases :
¡° Currently, I have been performing endoscopy of the stomach and colon using PENTAX Medical IMAGINA system for about 2 years. Previously, PENTAX Medical EPK-i video endoscope was used for examination. IMAGINA system exhibits more vivid colors and lighter handling, and it is easier to detect mucosal changes in close-up than any other system. In terms of color, images are reproduced without any visual burden, and this provides natural images when I explain the endoscopic findings directly to patients.¡°
Autoimmune Gastritis with Helicobacter pylori Infection
Patient History
A 77-year-old female patient visited hospital for a follow-up examination for gastric subepithelial tumor. She complained about intermittent indigestion and often felt lethargic and weakness. She was taking antihypertensive drugs and having no history of taking other gastric acid secretion inhibitors.
Patient's Laboratory Finding
| Serologic tests | Patient |
|---|---|
| Pepsinogen I | 12.9 |
| Pepsinogen II | 21.9 |
| Pepsinogen I/II | 0.6 |
| Gastrin (13 ~ 115 pg/mL) | 201 |
| Anti-H. pylori IgG (0.0 ~ 0.89 U/mL) | 4.28 |
| Anti-parietal cell ab. | Positive |
| Rapid urease test | Positive |
Endoscopic Findings & Treatment
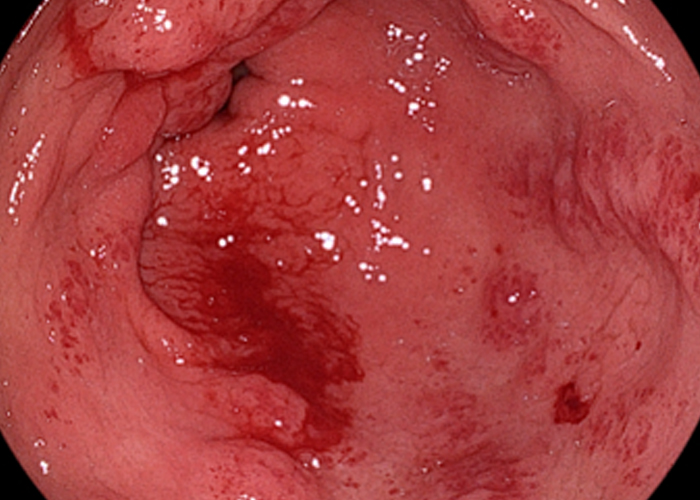
Endoscopy showed multiple whitish plaques with diffuse erythema from the antrum to the angle of stomach (Image 1, 2). Severe atrophic mucosa, changed with
prominent submucosal vascularity, was observed in the fundus and body (Image 3, 4). The degree of atrophy was observed more severely in the body than in the
antrum; therefore, endoscopic biopsy with forceps on the body and antrum respectively and then serologic test were performed together. In serology,
Anti-Helicobacter pylori antibodies showed a positive result of 4.28 U/mL. A rapid urease test was performed together with suspected intestinal metaplasia in the
antrum and diffuse erythema observed in the gastric antrum and body, which was confirmed as positive. A diagnosis is made as autoimmune gastritis combined
with Helicobacter pylori infection.
Patient Outcome and Follow-ups
Helicobacter pylori was eradicated, and regular endoscopy was recommended every 2 years.
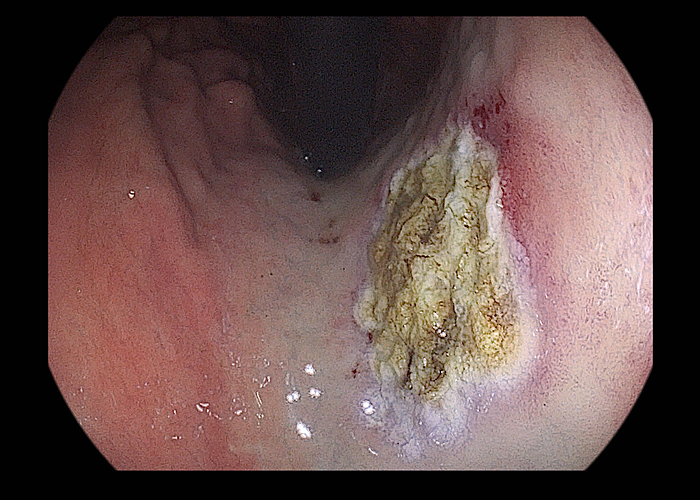
Image 1
Several small whitish plaques with some erythematous mucosa was observed on antrum
Image 2
Multiple whitish plaques, observed as intestinal metaplasia, were seen up to the gastric angle.
Image 3
Endoscopy performed by retroflexion and the severe mucosal atrophy
with marked vascular visibility observed in the body and fundus.
Image 4

The disappearance of folds without atrophic border is observed on the
entire area of the greater curvature in the body.
Summary
SUBMITTED
Thank you